What is new in DSM-5
What is new in DSM-5 for Schizophrenia Spectrum & other Psychotic Disorders; Bipolar & Related Disorders; Depressive Disorders; and Personality Disorders?
Going over what is new in the DSM-5 for Schizophrenia Spectrum & other Psychotic Disorders; Bipolar & Related Disorders; Depressive Disorders; and Personality Disorders.
Disclosures
- Grant Support from Genentech
- The grant is a naturalistic 5 year prospective study of 3000 patients with Schizophrenia
- The grant speaks to current state of research in Schizophrenia and the challenges in developing DSM 5
- Why are we doing a naturalistic study in 2013?
- Lack fine grained information about heterogeneity of Sz
- e.g. developmental course, prognosis, functional consequences, comorbidity, burden on family, caregivers, society
- Need this information to cross correlate with genetic and physiological measures
- Lack fine grained information about heterogeneity of Sz
DSM 5 represents incremental change, not transformational change
- The hope had been for a dimensional rather than categorical approach to diagnosis
- The construct was to apply genetic findings, neuro-imaging, physiological markers, and neuro-cognitive markers
- They would be cross correlated with dimensional environmental factors
- Nutritional, infectious disease, toxins, antigens, and psychosocial adversity
- Allowing for patient specific diagnoses rather than the categorical diagnoses of DSM IV
- The hope was not realized: here I review the incremental change found in DSM 5
Schizophrenia Spectrum and Other Psychotic Disorders
- Schizophrenia, > 6 months, > 1 month active-phase
- Schizotypal (Personality) Disorder
- Delusional Disorder
- Brief Psychotic Disorder, > 1day, < 1 month
- Schizophreniform Disorder, > 1 month, < 6 months
- Schizoaffective Disorder, some overlap of mood episodes (mood episodes occur > 50% of lifetime duration of illness) with psychosis and > two weeks
- Substance/Medication-Induced Psychotic Disorder
- Psychotic Disorder Due to Another Medical Condition
- Catatonia Associated with Another Mental Disorder (Catatonia Specifier)
- Catatonic Disorder Due to Another Medical Condition
- Other Specified Schizophrenia Spectrum and Other Psychotic Disorder
- Unspecified Catatonia & Unspecified Schizophrenia Spectrum and Other Psychotic Disorder
- Clinician’s choice and data may be insufficient
Schizophrenia Spectrum and Other Psychotic Disorders: Key Features
- Delusions
- Hallucinations
- Disorganized Thinking (Speech)
- Grossly Disorganized or Abnormal Motor Behavior, including Catatonia
- Negative Symptoms (simplified to 2 domains)
- Diminished Emotional Expression
- Avolition
Schizophrenia
- Elimination of special treatment of bizarre delusions and “special” hallucinations in Criterion A (characteristic symptoms)
- Rationale: This was removed due to the poor reliability in distinguishing bizarre from non-bizarre delusions.
- Schneiderian Delusions carry no special weight
- At least one of two required symptoms to meet Criterion A must be delusions, hallucinations, or disorganized speech
- Rationale: This will improve reliability and prevent individuals with only negative symptoms and catatonia from being diagnosed with schizophrenia.
- Deletion of specific subtypes
- Rationale: DSM-IV’s subtypes were shown to have very poor reliability and validity. They also failed to differentiate from one another based on treatment response and course.
- Eliminates:
- Paranoid Type
- Disorganized Type
- Catatonic Type (Catatonia becomes a specifier)
- Undifferentiated Type
- Residual Type
Schizophrenia 295.90 (F20.9)
- A. Active phase, 1 month of two or more, must include one * item
- Delusions*, hallucinations*, disorganized speech*, grossly disorganized or catatonic behavior, negative symptoms
- B. Deterioration and Impairment in work, interpersonal relations, or self care
- C. Duration, 6 months of negative symptoms or 2 or more Criterion A symptoms in attenuated form
- D. Rule out Schizoaffective and depressive/bipolar disorder with psychotic features
- E. Not due to drug abuse, medication, medical illness
- If history of autism or communication disorder of childhood, must meet criteria A – E.
Catatonia Associated With Another Mental Disorder (Catatonia Specifier)
293.89 ( F06.1)
- Now exists as a specifier for neurodevelopmental, psychotic, mood and other mental disorders; as well as for other medical disorders (catatonia due to another medical condition, e.g. cerebral folate deficiency, infections, metabolic, neurologic, rare autoimmune and paraneoplastic disorders)
- Rationale: As represented in DSM-IV, catatonia was under-recognized, particularly in psychiatric disorders other than schizophrenia and psychotic mood disorders and in other medical disorders. It was also apparent that inclusion of catatonia as a specific condition that can apply more broadly across the manual may help address gaps in the treatment of catatonia.
Catatonia Associated with Another Mental Disorder (Catatonia Specifier)
293.89 (F06.1)
A. Three or more:
- Stupor (no movement, unrelated to environment)
- Catalepsy (passive induction of a posture held against gravity)
- Waxy flexibility (slight, even resistance to positioning by examiner)
- Mutism (exclude if known aphasia)
- Negativisim (opposition or no response to instructions or external stimuli)
- Posturing (spontaneous maintenance of a posture against gravity)
- Mannerism (odd, circumstantial caricature of normal actions)
- Stereotypy (repetitive, abnormally frequent, non-goal-directed)
- Agitation not influenced by external stimuli
- Grimacing
- Echolalia (mimicking another’s speech)
- Echopraxia (mimicking another’s movements)
Catatonic Disorder Due to Another Medical Condition
293.89 (F06.1)
- A. three or more symptoms of abnormal movements, speech, or agitation (see prior slide)
- B. Evidence from Medical Examination due to direct pathophysiological consequences of another medical condition
- C. Not better explained by another mental disorder
- D. Not due solely to a delirium
- E. Distress or impairment in social, occupational, or other important functions
Schizoaffective Disorder
- Now based on the lifetime (rather than episodic) duration of illness in which the mood and psychotic symptoms described in Criterion A occur
- Rationale: The criteria in DSM-IV have demonstrated poor reliability and clinical utility, in part because the language in DSM-IV regarding the duration of illness is ambiguous. This revision is consistent with the language in schizophrenia and in mood episodes, which explicitly describe a longitudinal rather than episodic course. Similarly applying a longitudinal course to schizoaffective disorder will aid in its differential diagnosis from these related disorders.
295.70 (F25.0) Bipolar Type
295.70 (F25.1) Depressive Type
- A. Uninterrupted period of major mood episode (MDD or Bipolar) concurrent with Criterion A of Sz (overlap)
- B. Delusions or hallucinations for 2 or more weeks in the absence of a mood disorder during the lifetime duration of the illness (non over-lap)
- C. Major mood disorder present for > 50% of the active and residual lifetime duration of the illness
- D. Not due to medication, drug abuse, or medical illness
- Specifiers
- Bipolar, MDD, Catatonia
- First episode, Multiple episodes, Continuous
- Acute, degree of remission
Schizoaffective Disorder, research supports its inclusion as a schizophrenia spectrum disorder
- Unclear if it differs from Sz in terms of structural or functional brain abnormalities, cognitive deficits, or genetic risk factors
- Functioning and insight may not be impaired to the same degree as in SZ
- 1/3 as common as Sz, lifetime prevalence is .3%
- Prognosis somewhat better than Sz
- An initial diagnosis of Schizoaffective Disorder may change over time to Sz as the mood symptoms longitudinally occupy < 50% of the lifetime duration of the illness
Diagnosis-Specific Severity Assessment:
Symptom Domains for Schizophrenia
- Hallucinations
- Delusions
- Disorganized Speech
- Abnormal Psychomotor Beh
- Negative Symptoms
- (Restricted Emotional Expression or Avolition)
- Impaired Cognition
- Depression
- Mania
- 0 = Not Present
- 1 = Equivocal
- 2 = Present, but mild
- 3 = Present and moderate
- 4 = Present and severe
Attenuated Psychosis Syndrome
(categorized as a Condition for Further Study)
- May be a prodromal state; less severe and more transient than a psychotic disorder
- A. One of the following in attenuated form, with relatively intact reality testing
- Delusions
- Hallucinations
- Disorganized Speech
- B. Sxs present once per week for one month
- C. Sxs began or worsened in past year vs. SPD which is a relatively stable trait disorder of longstanding
- D. Sxs are distressing/disabling requiring a consult
- E. Not due to another condition or substance
- F. Does not meet criteria for another psychotic disorder
Attenuated Psychosis Syndrome: Risk and Prognostic Factors
- Temperamental prognostic factors associated with poor outcome and progression to psychosis
- Negative symptoms
- Cognitive impairment
- Poor functioning
- Genetic and Physiological Factors associated with poor outcome
- Family history of psychotic disorder(s)
- Structural, Functional, Neurochemical imaging data
Mania and Hypomania
(Bipolar and Related Disorders)
- Inclusion of increased energy/activity as a Criterion A symptom of mania and hypomania
- Rationale: This will make explicit the requirement of increased energy/activity in order to diagnose bipolar I or II disorder (which is not required under DSM-IV) and will improve the specificity of the diagnosis.
Mania and Hypomania
- “Mixed episode” is replaced with a “with mixed features” specifier for manic, hypomanic, and major depressive episodes
- Rationale: DSM-IV criteria excluded from diagnosis the sizeable population of individuals with subthreshold mixed states who did not meet full criteria for major depression and mania, and thus were less likely to receive treatment.
- “With anxious distress” also added as a specifier for bipolar (and depressive) disorders
- Rationale: The co-occurrence of anxiety with depression is one of the most commonly seen comorbidities in clinical populations. Addition of this specifier will allow clinicians to indicate the presence of anxiety symptoms that are not reflected in the core criteria for depression and mania but nonetheless may be meaningful for treatment planning.
Bipolar I Disorder, Manic Episode
296.xx (F31.xx)
- A. Abnormally and persistently elevated, expansive, or irritable mood and persistently increased goal-directed activity or energy, 1 week, 4 days if hypomanic, or any duration if hospitalized
- B. During episode three or more, four if mood only irritable:
- inflated self-esteem or grandiosity
- decreased sleep, e.g. 3 hours
- more talkative or pressured speech
- flight of ideas or subjective racing thoughts
- Distractibility
- increase in goal directed activity or psychomotor agitation
- activities with painful consequences: buying sprees, promiscuity, foolish investments
- C. Marked impairment, hospitalization, psychotic features are present
- D. Not due to drugs, medication, medical condition
- Mania induced by antidepressant, ECT, or other treatment that persists beyond the physiological effect of the treatment is considered Mania and counts for a BPD Dx
Coding and Specifiers for Bipolar I Disorder
- Severity: mild, moderate, severe
- Current or Recent episode manic or depressed
- Are psychotic features present?
- In partial or full remission
- Specifiers
- Anxious distress
- Mixed features
- Rapid cycling
- Melancholic features
- Atypical features
- Mood-congruent psychotic features
- Mood-incongruent psychotic features
- Catatonia
- Peripartum onset
- Seasonal pattern
Bipolar II Disorder, Hypomanic Episode, Distinguishing Features 296.89 (F31.81)
- 4 days duration
- Change in functioning
- Not marked impairment
- Not psychotic
- Not hospitalized
Coding and Specifiers for Bipolar II Disorder
- Severity: mild, moderate, severe
- Current or Recent episode hypomanic or depressed
- In partial or full remission
- Specifiers
- Anxious distress
- Mixed features
- Rapid cycling
- Mood-congruent psychotic features in depression
- Mood-incongruent psychotic features in depression
- Catatonia
- Peri-partum onset
- Seasonal pattern
Condition for further study: Depressive Episodes with Short-Duration Hypomania
- Meets criteria for Major Depressive Disorder at least once in lifetime
- Meets criteria for Hypomania at least twice in lifetime except that the duration of Hypomania is at least 2 days and less than four days
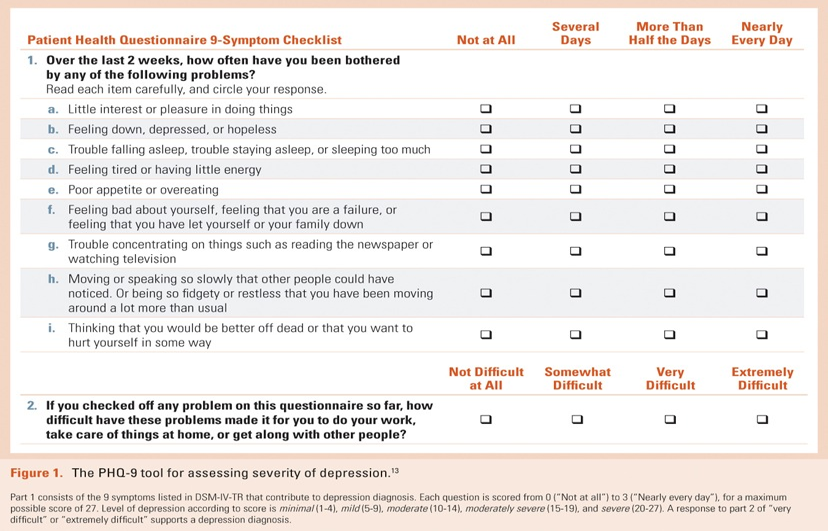
Diagnosis-Specific Severity Assessment:
PHQ-9, symptoms in Major Depression
Bereavement Exclusion
(Depressive Disorders)
- Eliminated from major depressive episode (MDE)
- Rationale: In some individuals, major loss – including but not limited to loss of a loved one – can lead to MDE or exacerbate pre-existing depression. Individuals experiencing both conditions can benefit from treatment but are excluded from diagnosis under DSM-IV. Further, the 2-month timeframe required by DSM-IV suggests an arbitrary time course to bereavement that is inaccurate. Lifting the exclusion alleviates both of these problems.
Bereavement Exclusion: expert clinical judgment is required
- “Although some depressive symptoms may be understandable or considered appropriate to the loss, the presence of a major depressive episode in addition to the normal response to a significant loss should be carefully considered. This decision inevitably requires the exercise of clinical judgment based on the individual’s history and the cultural norms for the expression of distress in the context of loss.” DSM-5, page 161
Personality Disorders (PD)
- All 10 DSM-IV PDs remain intact in Section II. However, Section III contains an alternate, trait-based approach to assessing personality and PDs that includes specific PD types (e.g., borderline, antisocial) but allows for the rating of traits and facets, facilitating diagnosis in individuals who meet core criteria for a PD but do not otherwise meet a specific PD type.
- Rationale: A hybrid model with both dimensional and categorical approaches is included in Section III. This model calls for evaluation of impairments in personality functioning and characterizes five broad areas of pathological personality traits. It identifies six PD types, each defined by both impairments in personality functioning and a pattern of impairments in personality traits. We will evaluate the strengths and weaknesses of the model, leading to greater understanding of the causes and treatments of PDs.
Alternative DSM-5 Model for Personality Disorders: General Criteria
- A. Impairment in functioning in 2 or more areas as uniquely specified in 7 subtypes
- Self
- Identity
- Self-direction
- Interpersonal
- Empathy
- Intimacy
- B. One or more pathological personality traits as uniquely specified in 7 subtypes
- Negative Affectivity vs. Emotional Stability
- Detachment vs. Extraversion
- Antagonism vs. Agreeableness
- Disinhibition vs. Conscientiousness
- Psychoticism vs. Lucidity
- C. Impairment and Traits present across most personal and social situations
- D. Impairment and Traits present since adolescence or early adulthood
- E. Not better explained by another mental disorder
- F. Not due to substance abuse, medication, or a medical condition
- G. Not normal for cultural group or developmental age
- Self
Specific Personality Disorders
- Antisocial
- Avoidant
- Borderline
- Narcissistic
- Obsessive-compulsive
- Schizotypal
- Personality Disorder-Trait Specified
- Made when a personality disorder is present but criteria are not met for a specific disorder
David L. Fogelson, M.D., www.DavidFogelson.com, June 2013; Copyright © 2013. American Psychiatric Association.
