Treatment Resistant Schizophrenia
David L. Fogelson, M.D. Clinical Professor of Psychiatry
David Geffen School of Medicine at UCLA And The Semel Institute for Neuroscience and Human Behavior at UCLA
Adapted from a PowerPoint Presentation created by Stephen Marder, M.D., 2018, used with permission
19 year old mute college student responding to internal stimuli
- She was unable to give an account of herself
- She was preoccupied with internal stimuli and unresponsive to questions
- Failed trials of aripiprazole, risperidone, olanzapine, haloperidol, lurasidone
- At initial visit switched to paliperidone LAI
- Six months of Rx with minimal response
- Clozapine initiated, titrated to 325 mg per day, level 650 ng/ml
- After 8 weeks smiling, articulate, spontaneous speech, psychosis and depression in remission
- After 30 months adaptive functioning is limited, not working, not going to school
- Initiated Adjunctive levomilnacipran 60 mg/day, 2 years ago with marked improvement
- Working 30 hours per week
- Living independently
- Exercising regularly
- Preparing her own meals
Prevalence of Treatment Resistant Schizophrenia (TRS)
- Some patients no initial response to treatment
- 10%-23% of patients have TRS from illness onset
- Patients may initially respond to treatments
- But 30%-60% become partially responsive or resistant to treatment!
Clinical Evaluation of TR
- Compliance is an over arching issue
- Early consideration should be given to depot preparations
- Early consideration should be given to switching if TR
- After 2 weeks at an adequate dose (super doses not required)
- TR is not only in the realm of psychotic symptoms, must assess and address:
- Evaluate social and vocational functioning
- Evaluate Depression
- Evaluate Cognitive Deficits
- Evaluate Disorganization
- Impairment in all these Sx realms constitutes TR
Early Response/Non-response at 2 weeks (Kinon et al 2010) is a guide whether to switch or not
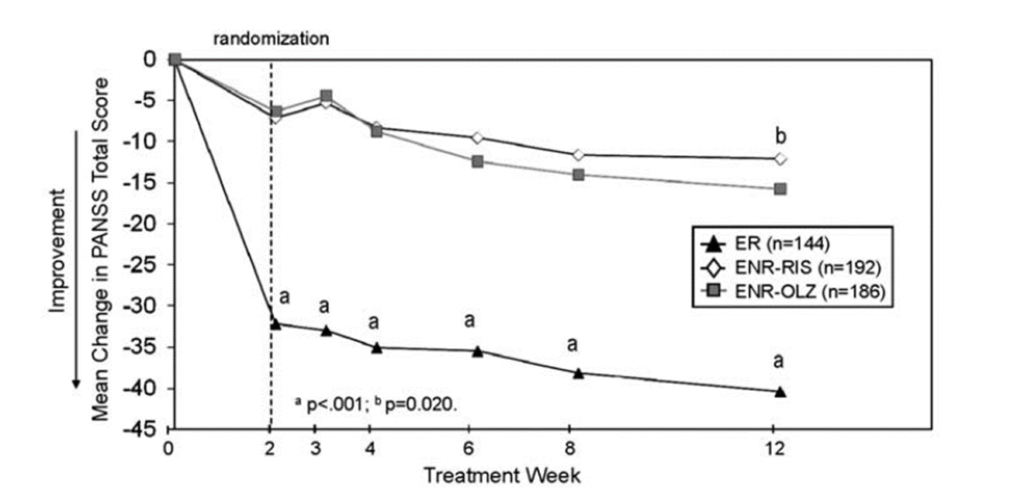
High Dosages outside therapeutic range are no more effective and may cause harm
- One exception
- If maximum therapeutic dose has been reached without side effects
- Must carefully evaluate EPS
- Must carefully evaluate other common side effects
- Constipation
- Cardiovascular Effects
- Metabolic Parameters
- Only then initiate a trial with high dose
- Monitor and review regularly—every week or two
- If no major improvement after three months return to standard dosage
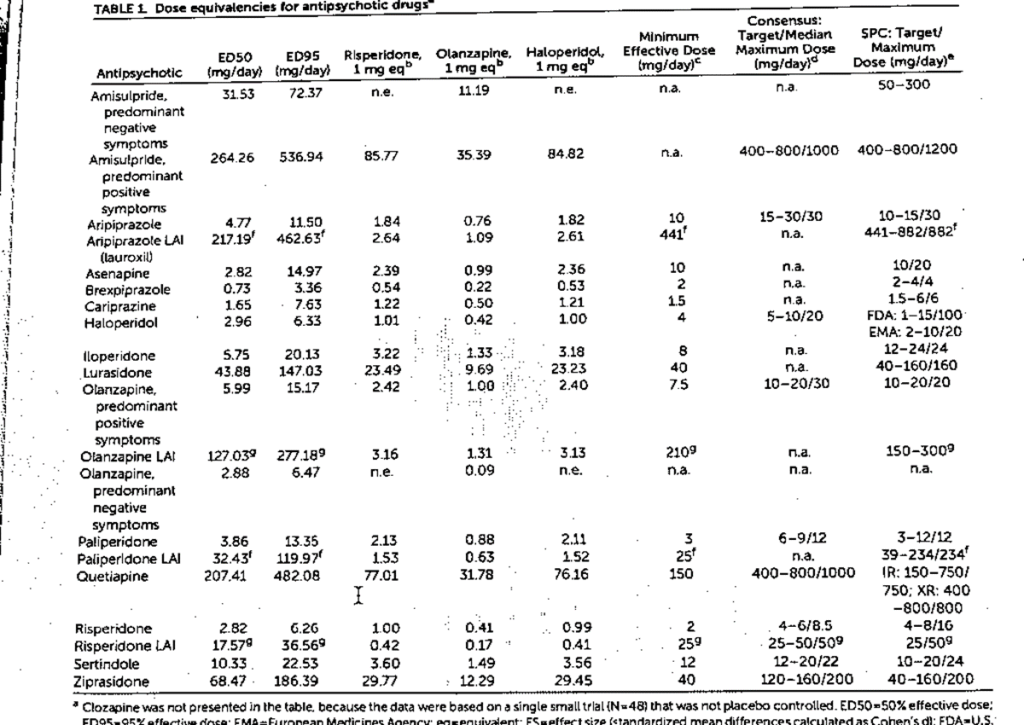
ED95 for Antipsychotic Meds
Leucht et al, Am J Psych, April 2020
Any Benefit to Combinations of Antipsychotics with another Med?
- Little evidence for combining one antipsychotic with another antipsychotic
- Little evidence for adding a mood stabilizer for symptoms other than mood symptoms
- I find AEDs and Lithium helpful in Schizo-affective, Bipolar patients
- I find Anti-depressants helpful for depression and negative symptoms; SNRI’s most effective
- These recommendations remain anecdotal
- Will review a Meta-analysis of this question later in lecture

From: Association of Antipsychotic Polypharmacy vs Monotherapy With Psychiatric Rehospitalization Among Adults With Schizophrenia
JAMA Psychiatry. 2019;76(5):499-507. doi:10.1001/jamapsychiatry.2018.4320
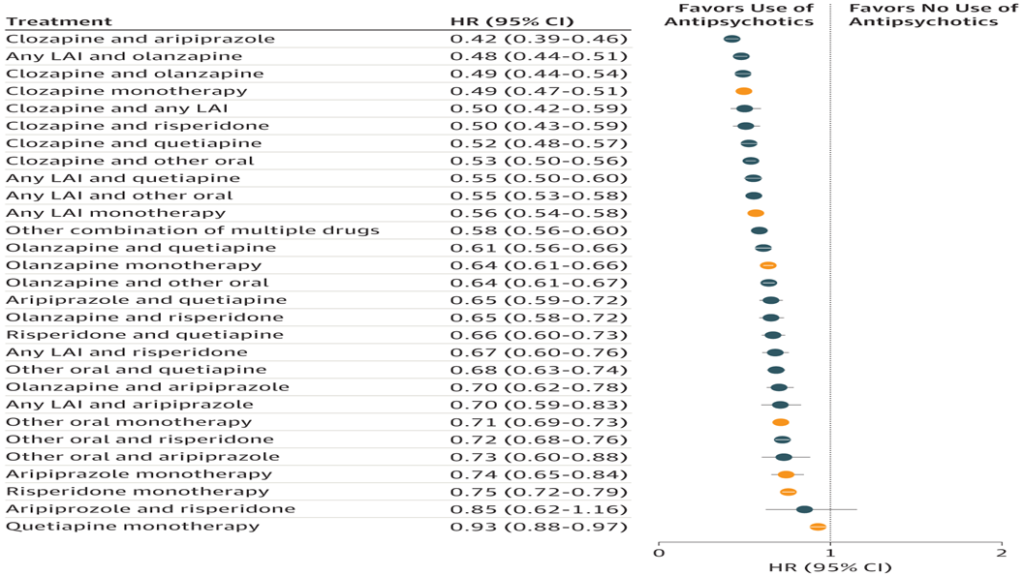
Risk of Psychiatric Rehospitalization During Specific Treatments Compared With No Antipsychotic Use in the Prevalent Cohort (Within-Individual Analysis) HR indicates hazard ratio; LAI, long-acting injectable agent. Orange markers indicate monotherapies.
From: Association of Antipsychotic Polypharmacy vs Monotherapy With Psychiatric Rehospitalization Among Adults With Schizophrenia
JAMA Psychiatry. 2019;76(5):499-507. doi:10.1001/jamapsychiatry.2018.4320
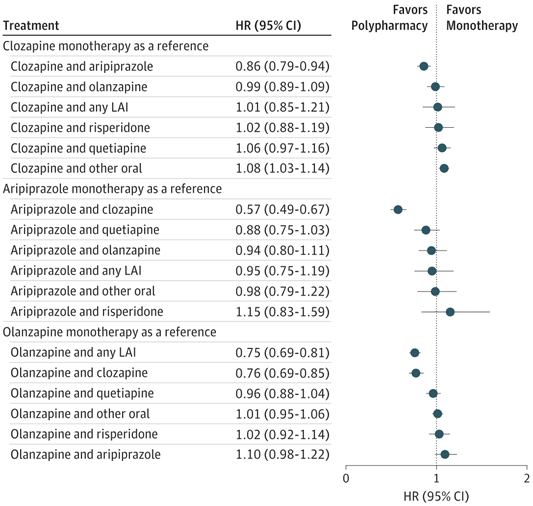
Figure Legend:
Risk of Psychiatric Rehospitalization in the Total Cohort, Compared With Clozapine, Aripiprazole, and Olanzapine Monotherapy (Within-Individual Analysis)HR indicates hazard ratio; LAI, long-acting injectable agent.
Date of download: 7/21/2020
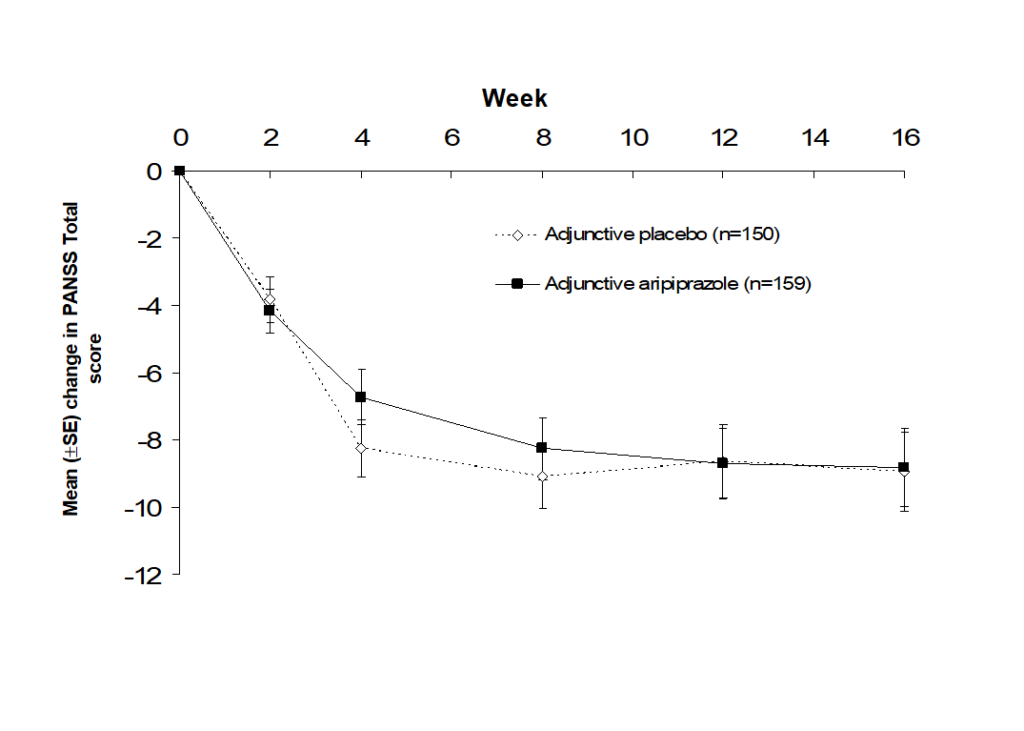
Aripiprazole does not augment Risperidone or Quetiapine (Kane et al 2009)
Does formulation matter? Oral v Long-acting Injectables Ostuzzi et al Sz Research 2017
- The authors present a literature review and meta-analysis
- Non-compliance is postulated to be a major factor in TRS
- The hope is that Long-acting preparations will overcome non-compliance resulting in much better outcomes
- The hope is not realized
- 18 studies (n=5,000) of risperidone, olanzapine, aripiprazole, zuclopenthixol, fluphenazine, haloperidol
- No advantage in terms of drop outs for any reason including ADRs
- No advantage in terms of efficacy
- This is counter to my anecdotal experience with non-compliant patients who have been switched from oral to LAI
- A Confounder is that in clinical trials the adherence to oral medication is better than in clinical practice
Comparative Efficacy of 15 antipsychotics: a multiple-treatments meta-analysis (Leucht et al, 2013)
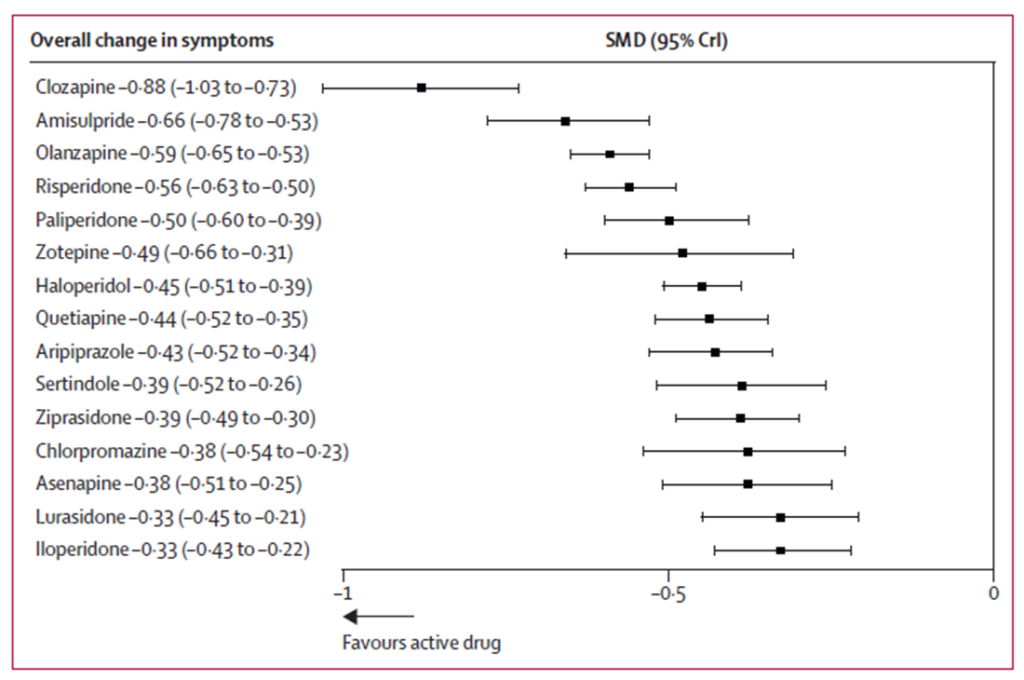
Clozapine, Clozapine, Clozapine!
- Clozapine has nearly twice the potency compared to the average oral AAP
- Who should receive Clozapine?
- Patients who have failed 1-2 trials of an AAP due to lack of efficacy
- Delay initiating clozapine should be < 1 year
- While depot AAPs are more effective than oral AAPs
- They may not be as effective as clozapine for positive symptoms, disorganization, and depression
- All Sx domains must be carefully evaluated
How do I dose Clozapine?
- Most patients will tolerate a minimum dose of 300 mg
- Most patients will receive a dose between 250-600 mg
- Most patients will tolerate a dose titration beginning at 25 mg and increasing by 25 mg per day to desired dose
- Plasma drug levels are a guide
- Lowest effective levels 250-550 ng/ml, trough level pre-dose
- Upper limit to prevent seizures, ileus, sedation: 600-2000 ng/ml
- Adequate trial is a minimum level of 350 ng/ml
- Hasegawa et al 1993, Spina et al 2000, Vander Zwaag et al 1996, Olesen 1998
- Dettling et al 2000. Schulte PFJ. Clinical Pharmacokinetics 2003;42:607-618
- Check a quantitative level after reaching 300 mg HS
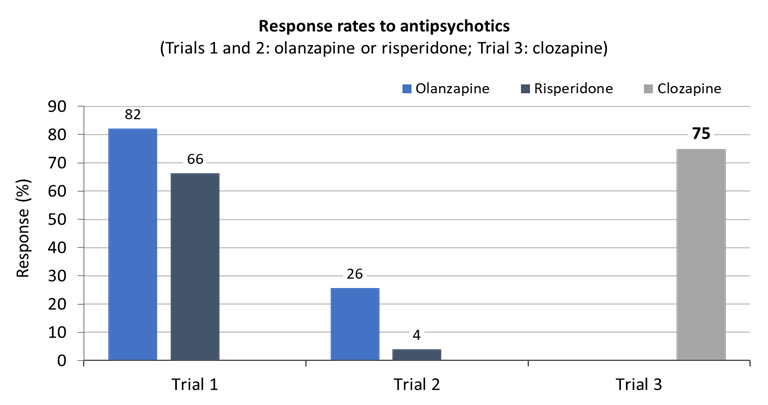
Clozapine Initiation, sooner than later for better Symptomatic Outcomes
In Japanese patients with TRS (2 failed trials, n=90), delayed initiation of clozapine was negatively correlated with symptomatic improvement, BPRS total score. Duration of illness not a factor.
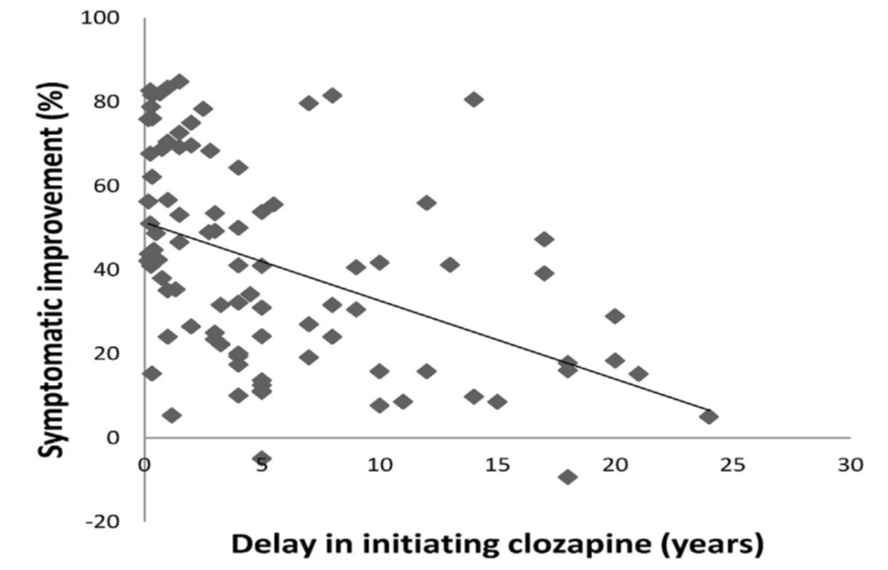
BPRS=Brief Psychiatric Rating Scale; rs=Spearman rank-order correlation coefficient.
Yada, et al. Schizophr Res. 2015;168(1-2):585-586.
Antipsychotic Treatment Prior to Clozapine Initiation in Community Settings
| Study | Country | Mean Number of Years Diagnosed Before Clozapine | Mean Number of Antipsychotics Used Before Clozapine |
| Howes, 2012 | UK | 4.8 | 3.9 |
| Nielsen | Denmark | 4.0 | N/A |
| Wheeler | UK (Birmingham Australia (Auckland) | 6.5 5.3 | 4.3 3.1 |
| Taylor | UK (London) | 5.0 | 5.5 |
| Alessi-Severini | Canada | 8.6 | 3.3 |
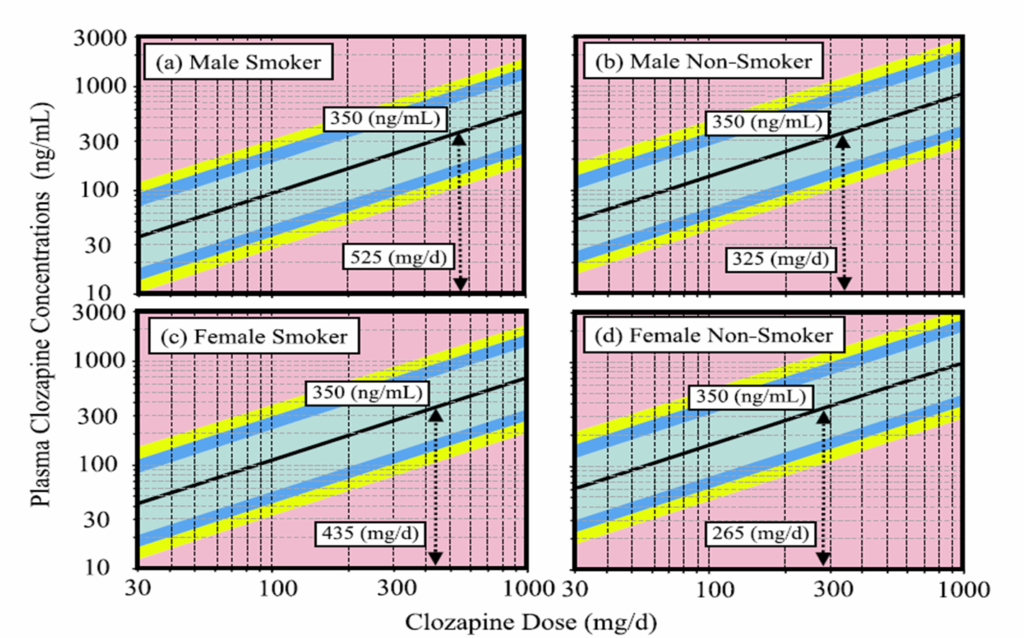
Nomograms showing the likelihood of observed plasma clozapine trough concentration for a given daily dose in a 40 year old patient with an average weight of 80 kg (male) or 70 kg (female) and a clozapine/norclozapine MR of 1.32
Rostami-Hodjegan et al. J Clin Psychopharmacol. 2004;24:70-8
ADEQUATE TRIAL OF CLOZAPINE
DURATION
- Period recommended varies from 4 to 12 months
- Meltzer 1992, Conley et al 1997
- Review of studies of plasma drug monitoring and the time to response, concluded an adequate trial should be at least 8 weeks
- Schulte 2003
- Response may be delayed longer in a proportion of patients: Meltzer 1992
- 6 weeks: 30% of patients will respond
- 3 months: another 20%
- 6 months: further 10–20%
- Reasonable to test clozapine monotherapy for 6 months
- Kerwin & Bolonna Adv Psychiatr Treat 2005;11:101–6
Efficacy of 42 Pharmacologic Cotreatment Strategies Added to Antipsychotic Monotherapy in Schizophrenia Systematic Overview and Quality Appraisal of the Meta-analytic Evidence, Correll et al
- Primary outcome was total symptom reduction. Secondary outcomes included positive and negative symptoms, cognitive and depressive symptoms
- 3397 publications, 29 meta-analyses testing 42 combination strategies in 381 individual trials and among 19 833 participants were included.
- Fourteen combination treatments outperformed controls
- No combination strategies with clozapine outperformed controls.
- Quality of the meta-analyzed studies was low
- Effect sizes were inversely correlated with meta-analyzed study quality, reducing confidence in these recommendations.
- no single strategy can be recommended for patients with schizophrenia based on data
- JAMA Psychiatry. 2017;74(7):675-684.
doi:10.1001/jamapsychiatry.2017.0624 Published online May 17, 2017
Which co-treatments cannot be endorsed?
- Antidepressants
- Mood Stabilizers
- Hormones
- Antioxidants
- Stimulants
- A second antipsychotic medication
What makes for a poor quality study?
- Small N
- results not confirmed by a larger trial
- Attrition and survivor biases, inflate positive outcomes
- publication bias was problematic resulting in overestimating effect size
- The overall quality of studies was inversely correlated with the effect size for total psychopathology
Stroup et al, Am Journal of Psychiatry, 2016
- National Medicaid Data was used to compare 3,123 pts initiated on clozapine with the same number of propensity matched pts started on other antipsychotics
- Clozapine resulted in decreased hospital admissions and decreased changes in antipsychotic, but increased rates of diabetes, hyperlipidemia, and intestinal obstruction
- Strategies for limiting side effects
- Excellent bowel care & judicious use of laxatives
- Miralax, Dulcolax, and Metamucil
- Education about exercise & nutrition
- Rx Metformin
- Monitor metabolic blood tests
- Excellent bowel care & judicious use of laxatives
Does treatment with any AAP medication lower mortality?
Tiihonen et al, Lancet, 2009
- Yes, well maybe
- Tiihonen concludes
- Long-term treatment with antipsychotic drugs is associated with lower mortality compared with no antipsychotic use
- Clozapine is associated with substantially lower mortality than any other antipsychotics
- Should restrictions on the use of clozapine be reassessed?
- What does a critical appraisal by De Hert et al in Schizophrenia Research, 2009, conclude?
Do antipsychotic medications reduce or increase mortality in Sz?
De Hert et al, Sz Research, 2009
- Methodological and conceptual issues make interpretation of these findings problematic
- incomplete reporting of data
- N per medication group, mean age, sex, duration of illness, duration of treatment, polypharmacy
- questionable selection of drug groups and comparisons
- e.g. 40% were in polypharmacy group, but no attempt to tease out individual drug effects
- important unmeasured risk factors
- Marital status, substance abuse, socio-economic status, habits, cardiovascular history
- exclusion of deaths occurring during hospitalization leading to exclusion of 64% of deaths on current antipsychotics
- survivorship bias due to strong and systematic differences in illness duration across the treatment groups
- incomplete reporting of data
- prospective mortality studies, with direct measurement of and adjustment for all known relevant risk factors for premature mortality, are needed
- Only then can we identify risk and protective medications
- Only then can we identify risk and protective patient factors
- Only then will we be able to inform clinical practice.
- Not a simple Yes or No, we just do not know!
- In the meantime
- Treat to alleviate suffering
- Treat to improve adaptive functioning
- Mitigate risks: habits, nutrition, exercise, prophylactic health monitoring
The Schizophrenia Patient Outcomes Research Team (PORT): Updated Treatment Recommendations 2009
Schizophrenia Bulletin
- Expert Panel
- 39 researchers, clinicians, and consumers
- 600 studies reviewed
- Medication and Psychosocial Intervention guidelines were promulgated
- This study was funded by
- The Agency for Healthcare Research and Quality (AHRQ)
- The National Institute of Mental Health (NIMH)
Schizophrenia PORT 2009
- After 2 failed trials of antipsychotic medication initiate a Clozapine trial
- An adequate trial of Clozapine
- At least 8 weeks in duration
- In a dosage range of 300-800 mg/day
- Optimize Clozapine Rx
- Trough blood level > 350 ng/ml
- Studies of simultaneous treatment with two or more antipsychotics (antipsychotic polypharmacy) show no > efficacy than monotherapy
Schizophrenia PORT – 2009
- AEDs and Lithium
- There is little evidence to support their use for TRS
- There is no recommendation that they should be used for TRS
Indications for Rx Clozapine
- Acute Sz
- Similar efficacy to other antipsychotics
- TRS
- Provides superior long term effectiveness
- Patients with TD
- Patients with comorbid Parkinson’s Disease
- Suicidal psychotic patients
- Treatment Resistant Mania
Clozapine Side Effects
- Sedation
- Hyperthermia
- Tachycardia, hypotension
- Please check vital signs, baseline EKG & as clinically indicated
- Metabolic Concerns; measure Hgb A1c, FBS, Lipid panel, weight
- Constipation; try to limit anticholinergic burden from other meds
- Please ask about bowel habits
- When was last BM
- What is the quality of BM’s, volume, texture, etc.
- What is frequency of BM’s
- Nausea and vomiting
- Seizures
- Sialorrhea; I do not recommend glycopyrrolate Rx as it exacerbates anticholinergic burden; atropine eyedrops 2 SL at bedtime may be helpful, minimal risk
- Urinary Incontinence: only Rx is adding pseudoephedrine, not recommended, risk for anxiety and psychosis
- Bone Marrow Suppression, details for monitoring in later slides
- Myocarditis, details for monitoring in later slide
- Please ask about chest pain, fatigue, dyspnea, tachypnea, fever, palpitations
REMS Program Required for Clozapine Rx
- A single registry (the Clozapine Risk Evaluation and Mitigation Strategy [REMS] Program, https://www.clozapinerems.com/).
- As part of REMS, clinicians need to be registered and demonstrate that they are competent to prescribe clozapine
- Physicians must review clozapine-related materials from the Clozapine REMS Program website and pass a knowledge test
Clozapine Monitoring of ANC; Frequency of CBC with diff count
- Before initiating therapy, ANC ≥ 1500/uL; > 1000/uL in BEN (benign ethnic neutropenia)*
- First 6 months, weekly monitoring, ANC ≥ 1500/uL or > 1000/uL in BEN, then go to every 2 weeks.
- 6 -12 months, every 2 week monitoring, ANC ≥ 1500/uL or > 1000/uL in BEN, then every 4 weeks.
- Mild Neutropenia, 1000 to 1499/ul, continue Rx, 3 times weekly until ANC > 1500/uL
- Once ANC ≥1500/μL, return to patient’s last “Normal Range” ANC monitoring interval
- Moderate Neutropenia, 500 to 999/uL, hematology consult, interrupt Rx, resume Rx once ANC > 1000/uL
- Daily until ANC ≥1000/μL, then
- Three times weekly until ANC ≥1500/μL
- Once ANC ≥1500/μL, check ANC weekly for 4 weeks, then return to patient’s last “Normal Range” ANC monitoring interval
- Severe Neutropenia, < 500/uL
- Do not re-challenge unless benefit outweighs risk
- Once ANC > 1000/uL, daily; Three times weekly until ANC ≥1500/μL, then resume treatment as a new patient under “Normal Range” monitoring
*Approximately 25% to 50% of persons of African descent and some ethnic groups in the Middle East have benign ethnic neutropenia, with low leukocyte and neutrophil counts.
Myocarditis and Clozapine
- Although the incidence of myocarditis is very low (approximately 2.8/100,000 patient-years), it has resulted in at least 17 deaths.
- Consider when there is unexplained fatigue, dyspnea, tachypnea, fever, chest pain, palpitations, and other evidence of cardiac failure
- If suspected: review Eosinophil count; order ESR, C-reactive protein, Troponins
- Increase in C-reactive protein (over 100 mg/L) and troponin elevation (greater than twice the upper limit of normal) reported to be 100 percent sensitive in detecting clozapine-induced myocarditis
Discontinuing clozapine
- Continue CBC monitoring for 4 wks
- If possible, avoid abrupt discontinuation
Rechallenging after discontinuation of Clozapine
- For neutropenia, consider, addition of lithium
- Successful rechallenge is rare for patients with full agranulocytosis
- Patients with severe neutropenia or agranulocytosis (ie, an absolute neutrophil count less than 500) should only be rechallenged if the harm from not using clozapine greatly outweighs the potential risks.
- Clozapine should be used with extreme caution, as many patients will quickly develop agranulocytosis again.
- Some reports of successful rechallenge after myocarditis
- Only rechallenge if harm from not using outweighs the risk
Cognitive Behavioral Therapy for TRS
- CBT for psychosis
- Cognitive Model of Psychotic Illness
- Psychotic experiences are common
- Reported by 40% of population
- Normals correct for odd experiences
- Normals are able to interpret the experiences as odd and relabel them
- Faulty appraisals are maintained by logical errors
- Psychotic experiences are common
- NIMH PORT recommendation
- CBT is indicated for residual psychotic symptoms
- Patient and therapist develop a shared understanding of the illness, identify symptoms, develop Cognitive and Behavioral strategies to correct for hallucinations and delusions
Cognitive-Behavioral Therapy for Medication-Resistant Psychosis: A Meta-Analytic Review (Burns AMN, et al. Psychiatr Serv. 2014;65(7):874-880)
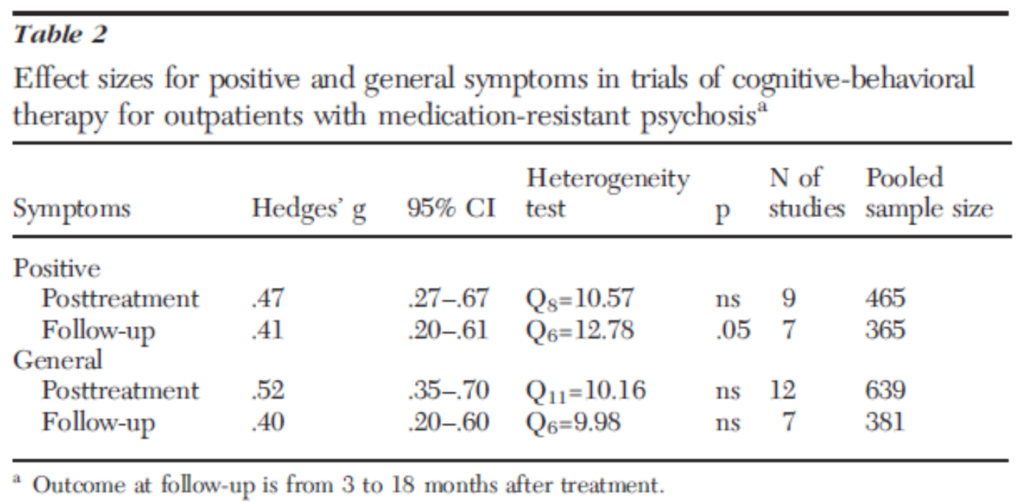
12 randomized controlled trials. N=639. 552 completed posttreatment assessment. These are medium effect sizes.
Editorial: Non-pharmacological Interventions for Schizophrenia: How Much Can Be Achieved and How? Andreou & Moritz, Front Psychol 2016
- Peters et al 2016 provide corroborating evidence that CBT is effective in routine delivery service venues, not just academic institutions.
- Mehl et al 2016 perform an updated meta analysis of CBT for delusions & confirm findings of Burns et al 2014, but indicate other psychotherapies may be equally effective
- Moritz et al 2016, So et al 2016, & Balzan 2016, report that metacognitive training addressing reasoning biases associated with emergence of delusions can
- Moderate bias
- Improve delusions
- Enhance Medication Compliance
- Other approaches with less evidence base include
- Social cognitive training
- Mindfulness training
- Family Therapy
- Future Directions: psychotherapy directed at depression and social anxiety
Transcranial Magnetic Stimulation (TMS) for Sz Cochrane Schizophrenia Group 2015
- TMS has been proposed as a Rx for TRS, especially for AH
- Compared TMS to sham TMS & to other interventions
- 41 studies with 1473 participants
- Results
- Temporoparietal TMS improved CGI (very low quality of evidence), improved + Sxs (very low quality); no evidence for improvement in cognition
- Prefrontal TMS did not improve global function; could not evaluate effect on + Sxs; no improvement in cognition
- Both Rxs caused more headaches than comparison Rx
- Conclusions
- Insufficient Evidence to support or refute effectiveness
- Evidence was not unequivocal
- No evidence that TMS was an effective adjunct to medications
- Overall quality of clinical trials was poor
- Risk of bias in ratings was present
- Number of subjects was small
- No standard for stimulation intensity, stimulation length, brain targets
- No standard scales used between studies
- Need standardized treatment protocols and measures for future studies to allow meta-analyses
Electroconvulsive Therapy Added to Non-Clozapine Antipsychotic Medication for
Treatment Resistant Schizophrenia: Meta-Analysis of Randomized Controlled Trials
Zheng W Plos One 2016
- Radomized Controlled Trials of ECT & Antipsychotic Med
- 11 studies, n=818, 10 weeks in duration
- ECT was superior to monotherapy with a medium effect size
- Symptom response as early as day 10
- NNT 6
- ADRs: headache and memory impairment
- Mean # of ECT Rxs 14
- Bilateral Lead Placement
- Caution: no data on neurocognitive outcomes
EAugmentation of clozapine with electroconvulsive therapy in treatment
resistant schizophrenia: A systematic review and meta-analysis Lally et al Sz Res 2016
- Five clinical trials, 71 patients
- Retrospective studies, 192 patients
- Overall response of 66% to ECT
- Mean # of ECT Rxs 11
- 32% relapse rate after discontinuation of ECT, f/u as long as 9 years
- Only one trial was a RCT
- Further research is needed before ECT augmentation can be included in clinical treatment of TRS
Summary
- Changing to another non-clozapine antipsychotic is sometimes effective
- High doses, combining antipsychotics, and adding mood stabilizers are seldom effective
- Delaying clozapine can have long-term consequences
- CBT and other psychosocial treatments are effective adjuncts
- ECT has demonstrated effectiveness for partial responses to clozapine and other antipsychotics