Diagnosis and Treatment of Major Depression in Adolescence
David L. Fogelson, M.D.
Clinical Professor of Psychiatry
David Geffen School of Medicine at UCLA
And The Semel Institute for Neuroscience and Human Behavior at UCLA

Mary
- Presents with frequent school absences
- Stomach aches
- Difficulty sleeping due to stomach pain
- Missing school frequently
- Sad nearly all the time
- Recent onset of the following symptoms
- Can’t sleep at night
- Not eating well
- Can’t concentrate at school, drop in grades
- Tired
- Feels worthless
- Thoughts of death and suicide

- Is Mary suffering from:
- A. Major Depression
- B. Dysthymic Disorder
- C. A depressive adjustment Disorder
- D. None of the above
- Answer a.
Clinical Depression: Major Depression
| Duration | ≥ 2 weeks |
| Critical Symptoms | Depressed, irritable , or anhedonic mood nearly all the time |
| # Symptoms- 5 of 9 symptoms must include depressed/irritable mood or anhedonia | Depressed/Irritable Mood Anhedonia Insomnia or hypersomnia Appetitie disturbance Concentration problems/indecision Low energy or fatigue Worthlessness or guilt for no reason Agitation or moves more slowly than usual Thoughts of death or suicide |
| Severity | Distress or functional impairment |
| EXCLUSION | Not due to drugs/medication/medical disorder. Not bereavement, not a mixed episode |
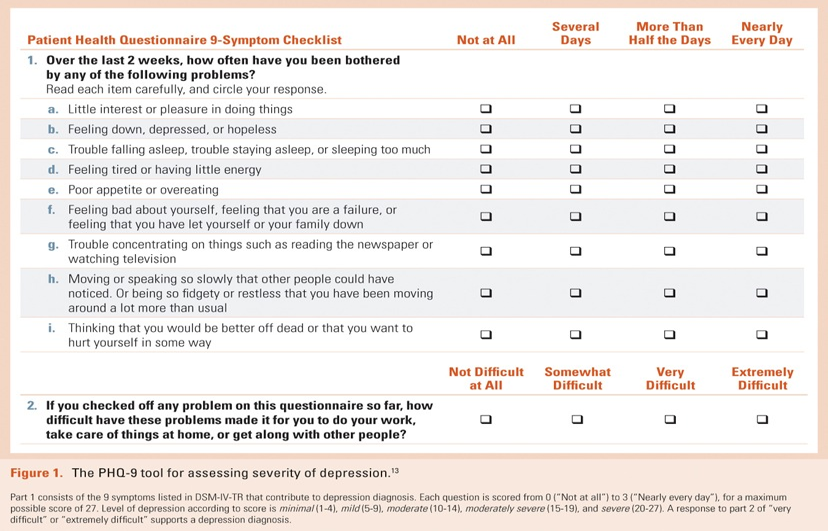
Diagnosis-Specific Severity
Assessment: PHQ-9, symptoms in
Danny
- Getting into trouble at school
- Irritable and crabby at home, been generally unhappy for past year
- Complains of being bored all of the time
- Feels like not as good as other kids
- Can’t concentrate in school, drop in grades
- Says his life is awful, no reason to think it will get any better, feels like giving up

Does Danny suffer from:
- A. Major Depression
- B. Dysthymic Disorder
- C. Bipolar Disorder
- D. Oppositional Defiant Disorder
- E. None of the above
Answer b.
Clinical Depression: Dysthymic Disorder
| Duration | ≥1 year for children |
| Critical Symptoms | Depressed/ irritable mood most of the time more days than not |
| # Symptoms- 2 of 6 symptoms, must include depressed/irritable mood | Either overeating or lack of appetite. Sleeping too much or having difficulty sleeping. Fatigue, lack of energy. Poor self-esteem. Difficulty with concentration or decision making. Feeling hopeless. |
| Severity | Distress or functional impairment |
| EXCLUSION | No MDD in Year 1. Never manic/hypomanic/mixed/ cyclothymicNot due to psychosis, drugs/medication/medical disorder. Not bereavement |
Ana
- Presents to ER with suicide attempt, serious overdose
- Boyfriend broke up with her
- Hasn’t been able to stop crying since break-up 5 days ago
- Feels worthless
- Can’t sleep
- Doesn’t feel like eating
- Worried that she is pregnant, feels nauseous
Anna suffers from Major Depression.
Depression is
- A. Extremely rare in teens, <.1%
- B. Rare, < 1%
- C. Low frequency, 1-2%
- D. Common, 5-6%
Answer D
Children do suffer from depressive disorders:
Pediatric depression is a prevalent condition
- Rates increase with age; pattern differs by gender
- <13 yrs: 2.8% (+ .5)
- 13-18 yrs 5.6% (+ .3)
- 1:1 sex ratio (or more boys) prior to adolescence
- Increased frequency in girls during adolescence
- 13-18 yrs girls 5.9%
- 13-18 yrs boys 4.6%
- Rates approach adult prevalence by end of adolescence
After the first episode of depression remits the risk for a second episode is approximately:
- a. 10%
- b. 30%
- c. 50%
- d. 70%
Answer c.
Pediatric Depression Not Benign Condition
- Depression recurrent (in up to ~60-75% of cases),
- 20% have persistence >2yrs
- 40-60% relapse after successful treatment
- 70% have adult depression
- Episodes are lengthy: MDD (7-9 mos) in clinical cases; Double Depression (~3yrs)
- Associated with significant impairment in school, with family, and peers
- Suicide risk in adults with history of adolescent MDD is 5x adults with late onset
Elevated rates of Suicide & Suicide Attempts in Adolescent-Onset MDD
by Early Adulthood
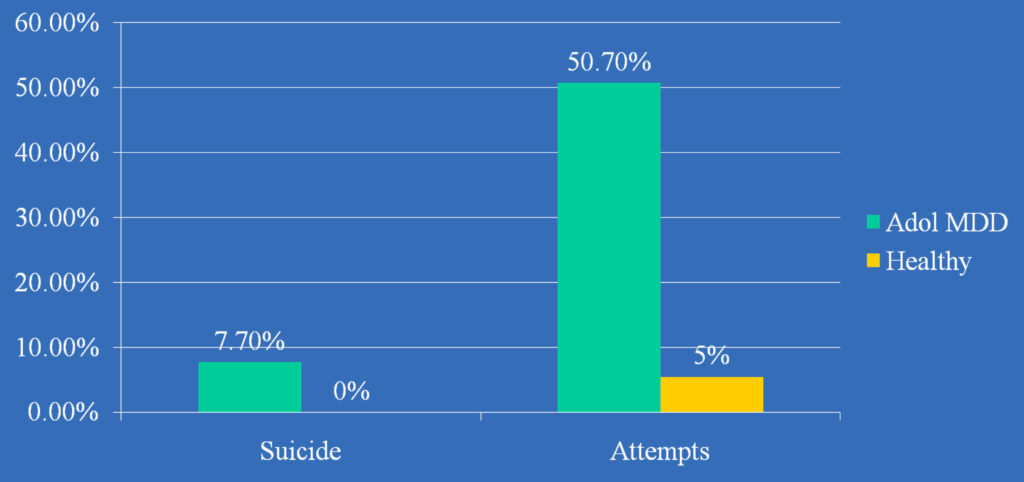
From Weissman et al. (1999). Depressed Adolescents Grown Up. JAMA
Mean age at follow-up 26 yrs, follow-up period ≈10 years
Comorbidity/Co-Occurring Disorders: High Across Range of Disorders
- Most youths present with another diagnosis, ~80-90%
- 40-50% have an anxiety disorder, anxiety disorders often precede the onset of depressive disorders
- Double depression common, ~ 20% DD/MDD
- ADHD comorbid in ~ 20%
- Conduct disorder in ~ 50% of school age depressives
- Increased risk for bipolar disorder (8%-49%)
- Common overlap with PTSD, OCD
Baji et al., in press; Biederman et al., 1995; Carlson & Kashani, 1988; Ferro et al., 1994; Fombonne et al., 2001; Geller et al., 2001; Goodyer et al., 1997; Kovacs et al., 1988/89, 1994, 1997 and Unpub; McCauley et al., 1993; Mitchell et al., 1988; Rao et al., 1995; Ryan et al., 1987; Shain et al., 1991; Strober & Carlson, 1982; Strober et al., 1993; Weiss & Garber, 2003; Weissman et al., 1999a,b
TREATMENT
Do we have effective treatments?
Treatment for Depression in Children and Adolescents
- Psychotherapy
- Pharmacotherapy
- Combination psychotherapy and pharmacotherapy
Studies in Children and Adolescents indicate that the most Effective treatment for Depression is:
- A. Psychotherapy
- B. Pharmacotherapy
- C. Combination Psychotherapy and Pharmacotherapy
- D. None of the above are better than placebo
answer c.
Fluoxetine Treatment for Depression in Children and Adolescents
Remission Rates
- Fluoxetine 41%
- Placebo 20%
p<0.01; Emslie GJ, Heiligenstein JH, Hoog S, et al. J Am Acad Child Adolesc Psychiatry. 2000
Drug Treatments for Child and Adolescent Depression: Levels of Evidence
| Short-Term Efficacy | |
| Fluoxetine Sertraline Fluvoxamine Paroxetine Citalopram/Escitalopram TCAs Venlafaxine Duloxetine | A * B C B A * C B C |
Because meds pose a risk for suicide, they should:
- A. Never be prescribed
- B. Monitored carefully during the first month of treatment
- C. Avoided in Bipolar Depression
- D. B & C are correct
Answer d.
A = >2 randomized, controlled studies; B = 1 randomized, controlled study; C = Clinical experience (open studies, case reports, etc)
*– fluoxetine FDA approved for depression ≥ 8 yrs; Escitalopram > 12-17. Adapted from Jobson KO, Potter WZ. Psychopharmacol Bull. 1995;31:457–459.
Adapted from McCracken, 2009
FDA Public Health Advisory March 2004
Suicidality in Children and Adolescents Treated With Antidepressant Medications
Today the Food and Drug Administration (FDA) directed manufacturers of all antidepressant drugs to revise the labeling for their products to include a boxed warning and expanded warning statements that alert health care providers to an increased risk of suicidality (suicidal thinking and behavior) in children and adolescents being treated with these agents, and to include additional information about the results of pediatric studies.
What kind of depression treatment do teens prefer?
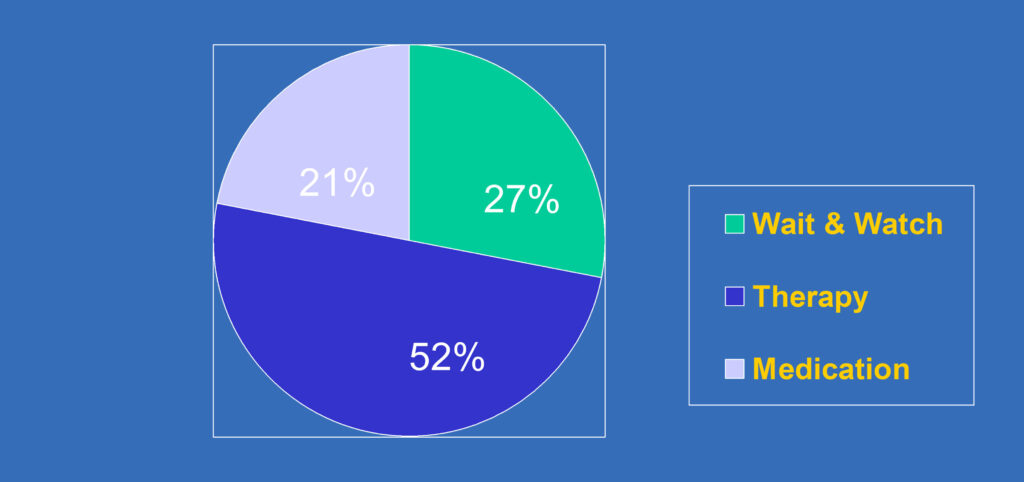
Jaycox, L.H., Asarnow, J.R, Sherbourne, C.D., et al. (2006). Adolescent Primary Care Patients’ Preferences for Depression Treatment. Administration and Policy in Mental Health 33, 198-207.
© Joan R. Asarnow for YPIC Team
Cognitive Behavior Therapy (CBT)
- Established psychosocial treatment for adolescent depression with evidence based supporting efficacy
- Acute treatment studies demonstrate greater efficacy for CBT (12-16 sessions) as compared to alternative psychosocial interventions and waitlist conditions
- Response rates for CBT appear to be between 60-66% (vs. 38-48% in comparison conditions)
- Although we focus on CBT today, there are accumulating data supporting other psychotherapies (e.g. IPT)
Psychotherapy Trial: MDD Remission
(No MDD + BDI <9 for 3 Weeks)
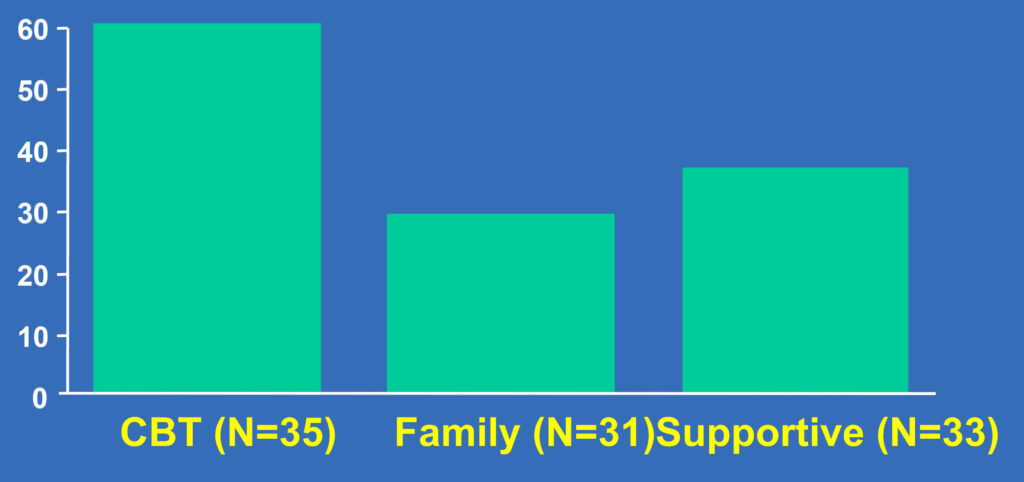
Overall p=0.05; CBT vs. family p=0.03; CBT vs. supportive p=0.04
Brent DA, Holder D, Kolko D, et al. Arch Gen Psychiatry. 1997(Sep);54(9):877-885
Courtesy, McCracken, 2009
Adolescent Depression
Combined CBT + Medication Treatment of Choice for Moderate to Severe Major Depression
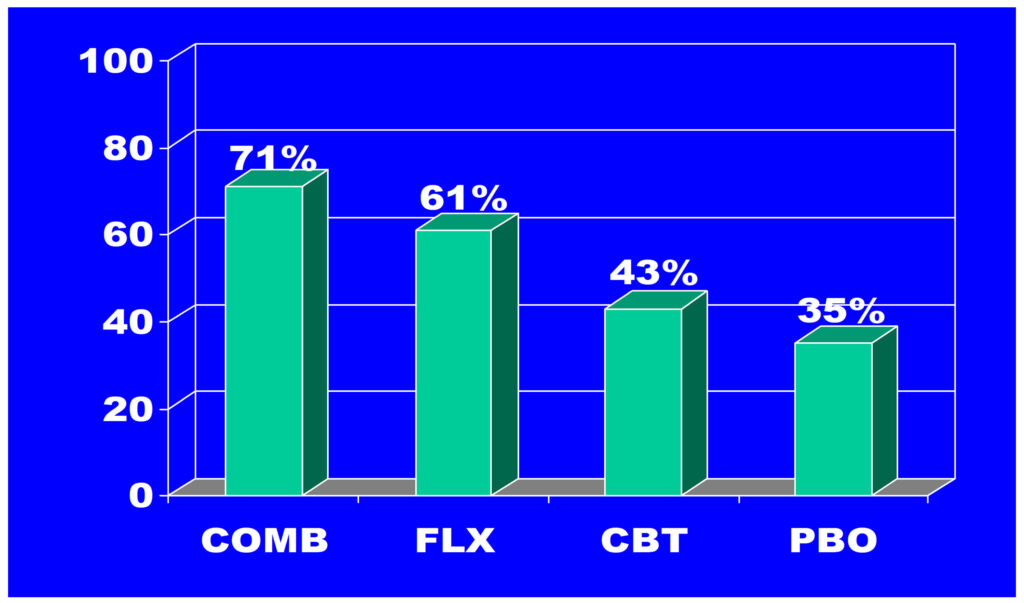
N=439, Treatment of Adolescent Depression Study (TADS); Week 12 Acute Treatment Response
TADS Recovery Incomplete: Remission Rates are Low & 50% of Remitted Youths Had Residual Symptoms
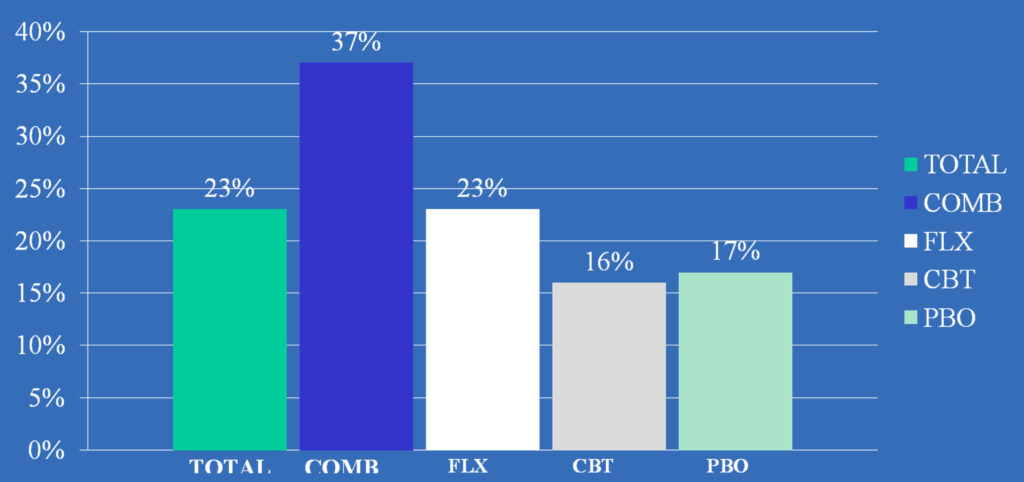
*CDRS-R total score ≤28 as the criterion for remission. COMB> FLX,CBT, PBO, P=.0009; FLX=CBT=PBO
Kennard et al. Remission and residual symptoms after short-term treatment in the Treatment of Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006 Dec;45(12):1456-60
6-Site NIMH Study
MH61835 Pittsburgh, Brent MH61864 UCLA, Asarnow MH61856 Galveston, Wagner
MH61869 Portland, Clarke
MH61958 Dallas, EmslieMH62014 Brown, Keller
- 334 outpatient adolescents, ages 12-17 years, with diagnosis of major depression
- Depression persists despite at least 6 weeks of SSRI treatment
- Acute phase 12-week trial
JAMA Feb 27, 2008
TORDIA Supports Value of CBT-Clinical Response by Treatment Group
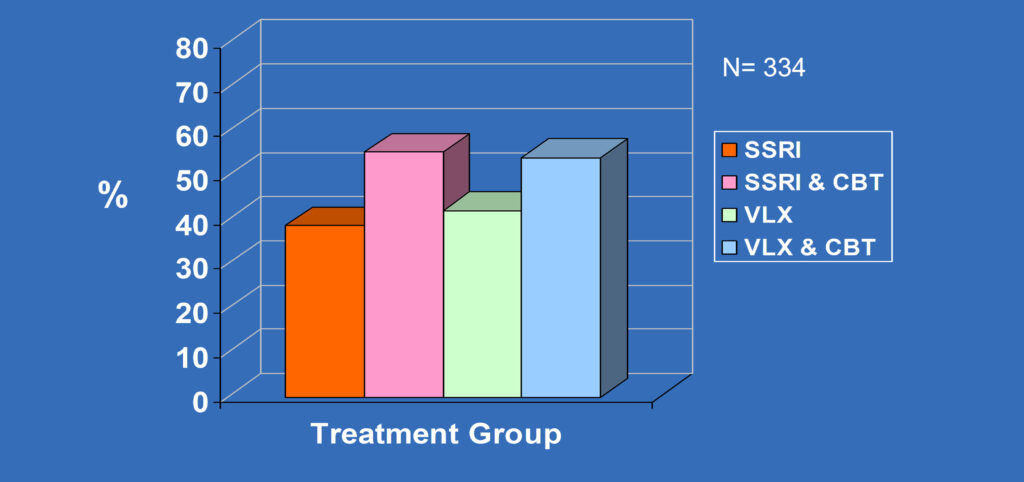
CBT vs none, 54.8% vs 40.5%, p<0.009
JAMA Feb 27, 2008